Reviewed by Jennifer Broxterman, MSc, RD
I never thought I’d be a “normal” eater.
For a long time, my best hope at peace was to keep my kitchen empty. Just a few staples so I had breakfast in the morning, and maybe dinner at night.
Because it felt like everything was a trigger food.
I would stand in front of my cupboard eating—get this—dry oats by the handful, jaw working furiously, like a horse.
I ate carrots—pounds—like I was mad at them, snapping their bodies viciously, anger-chewing them to pulp, stuffing them into my belly.
I would eat peanut butter in ice cream scoops, or frosted high on top of rice crackers.
Forget baking cookies. I would ruin the cozy ritual by eating the whole tray.
I was always hungry.
Actually, I was full—impossibly full—but I always wanted more.
I wanted to stop.
(Oh man, I wanted to stop.)
I wondered how “normal” people could keep food in their house: tins of cookies untouched for weeks, jars of peanut butter that lasted longer than two days.
It was inconvenient, and I felt like a freak.
I didn’t know how to climb out.
Until I did.
It took a good six or seven years of experimenting and failing, but eventually—clumsily, and definitely not magically overnight—I changed into a person I never thought I’d be:
A person whose thoughts weren’t constantly occupied by food.
A person who stopped viewing themselves as a collection of flesh-lumps to be compared and controlled.
A person who found a home in their body.
Below, I’ll share six steps that helped me recover from binge eating.
While writing this story, I also consulted with Jennifer Broxterman, MS, RD, a registered dietitian and PN Certified Coach who specializes in eating disorder recovery, and Ary Maharaj, M.Ed., a registered psychotherapist who facilitates a therapy group out of Sheena’s Place, a support center for eating disorders in Toronto, Canada. Their insights are woven throughout this article.
While this advice doesn’t replace the care of a health professional, we hope it provides you with an inkling of a path forward, and a sense of hope.
I never thought I’d get to where I am, honestly. But I’d like to tell you how I did.
Step #1: I came out of hiding.
My recovery started when I cracked the door open and let another person peer in.
Her name was Sarah.
We weren’t particularly close. We got along well, confided in each other about our crushes, but mostly, we studied together.
Both Psychology majors, we shared Abnormal Psychology and Statistics classes. As we practiced our ANOVA calculations, one day I told her.
“Sometimes I binge eat,” I said, testing.
Her reaction shocked me.
“Oh yeah, I do that. Like when I’m sad or stressed, I’ll eat everything,” she said without taking her eyes off her graph paper, as if she were telling me where she’d picked up her morning coffee.
I sat quietly.
I didn’t say more, but I let a feeling wash over me: relief.
I felt less alone, less weird. And strangely, accepted.
If someone else could receive this piece of information without running away, maybe I could stay and look at it a little closer too.
Try it yourself
If you’ve been hiding your eating behaviors from others, you’re probably doing it for a good reason.
This stuff is hard to share. It’s vulnerable, and people who binge often carry shame around this habit.
Unfortunately, hiding is shame’s favorite place to grow, and shame tends to perpetuate binge and comfort eating.1, 2
Consider who in your life you trust with sensitive information—a coach, a friend, a doctor—and tell them what you’ve been going through. Alternatively, consult the “Think you might need help?” box at the end of this article for resources and support.
Step #2: I stopped dieting and restricting.
Wait a sec… seems like my “problem” was eating too much, not too little, right?
Initially, that’s what I thought too.
However, in reality, the root of my struggle with food was restriction.
For months at a time, I’d control my calories, eat a lot of tuna and low-fat salad dressing, and lose weight.
Then I’d inevitably rebound, eating everything in sight.
When the binge was over, I would feel ashamed and pledge to undo the damage by dieting harder. And so the cycle continued.
What I didn’t know at the time?
Overeating is a natural response to undereating.
When I plowed into jars of cashew butter after weeks of controlled portions, it wasn’t my willpower that was failing; it was my biology winning. My body was just trying to keep me alive.
According to Broxterman, dieting and food restriction are known triggers for binge eating.
“Humans are hardwired to not die of famine. When food is chronically unavailable, all our senses become acutely attuned to finding, then consuming, as much food as possible. After periods of restriction, we are basically designed to binge to compensate.”
Once I recognized that binge eating nearly always followed restriction, I made a rule:
No more letting myself get hungry.
I promised myself I would have three square meals every day, plus two or three snacks spread out.
Through speaking with Broxterman, I learned my approach was similar to a strategy called mechanical eating, where you eat at regular intervals throughout the day, regardless of how you’re feeling physically or emotionally. (It’s often suggested when a person has lost touch with their natural hunger and fullness cues through chronic dieting or disordered eating.)
With a routine of square, satiating meals, my urge to binge plummeted.
I felt uncomfortable about eating regular, full meals, but I also felt hugely relieved to see the violent swings between extreme hunger and epic binges diminish.
Yes, I felt worried that eating regularly would cause me to gain weight. But I knew weight loss couldn’t be the ultimate goal anymore; love and care was.
Try it yourself
Mechanical eating aims to re-establish a reliable routine of eating balanced meals and snacks, as well as a connection to your hunger and fullness cues.
In general, mechanical eating requires that you eat 3 meals and 3 snacks spread out throughout the day, with roughly 3 hours between eating. (It’s sometimes referred to as “the rule of 3s.”)
Here’s what that looks like:
- Within the first hour of waking, eat breakfast.
- About 3 hours after breakfast, eat a snack.
- About 3 hours after your morning snack, eat lunch.
- About 3 hours after lunch, eat an afternoon snack.
- About 3 hours after your afternoon snack, eat supper.
- About 3 hours after supper, eat a bedtime snack.
In terms of amounts, you can use a tool like our Nutrition Calculator (select the “Improve health” goal), which can help you figure out how many portions of protein, carbohydrate, fat, and fruit/vegetables you should get, and how to spread them out throughout the day.
Step #3: I slowed down.
It’s hard to describe the urge to binge, although I think anyone who’s dealt with strong compulsions can relate:
It’s an itch, a Siren’s call, a little monkey in your brain tap-tapping, disrupting your resolve. It’s that game where someone tells you, “Don’t think of an elephant” and then all of a sudden, your brain is only thoughts of gray wrinkled knees, feathered black eyes, a heavy swinging trunk.
I would get the urge to EAT, to compete in a pie-eating contest, with no one watching. And that urge—like a horrible case of tinnitus—wouldn’t quiet until I binged.
When I started to eat regular meals and snacks, the craving-tinnitus quieted. But occasionally, I felt like the noise was too loud, and I just needed a “fix.”
So I made another rule:
If I really, truly couldn’t stop myself from bingeing, I would let myself. But I had to sit down, use plates and cutlery, eat slowly, and enjoy it.
Binges are often characterized by fast, distracted, frenzied eating.
In my case, I would stand in front of the fridge, or the cupboard, and use my hands—whatever tool was most readily available—to shove food into my mouth.
“In a typical binge, most people find that their brains and bodies go ‘offline.’ They disconnect from their thoughts, feelings, and body sensations as they wolf down food,” says Broxternman.
“So, slow eating introduces something new into the binge eating episode that’s usually turned way down: AWARENESS.”
Slow eating prevented me from numbing out while eating.
When I stopped using food as an anesthesia, all the feelings and thoughts I’d been avoiding came up. All my emotions were at the table, like a loving but dysfunctional family: comfort, emptiness, boredom, antsiness, loneliness, hope.
It was a lot to deal with, especially at first. But soon I realized, dealing with them was better than the futile effort of trying to stuff them down.
Try it yourself
Next time you get the urge to binge, just notice it. “I feel like I need to binge,” you might say to yourself inwardly or out loud.
If you feel like the binge is an unstoppable train, just lay out your tracks for a smoother ride:
First, serve yourself some food. A portion of whatever you want, to start.
Then, sit down at the table.
Pause, and maybe take a few deep breaths. Is it uncomfortable to not dive in right away? It’s okay. You’re handling it.
Now, take your first bite, and—revolutionary!—put your utensils down.
Take another breath.
Chew. Chew. Chew.
Pay attention to the taste and texture of your food. Enjoy it, even.
Relax.
Wait a few more moments before picking up your utensils again.
Repeat.
That’s it.
Sounds simple, but if you’re used to eating quickly—even if you don’t identify with bingeing—the above might be uncomfortable to read, let alone practice.
Eating slowly means you have to pay attention, and actually feel the sensations that emerge from your heart and body and mind.
(Gulp.)
However, all the feeling is WHY this tool works. You’re slowly taking away food’s power, because food can no longer serve as an emotional escape hatch.
Your feelings will have to find another place to go. That’s a good thing.
Step #4: I developed my tolerance for icky feelings.
I hadn’t realized how, over the years, food had become such a panacea for me: I ate when I felt bored, worried, lonely, excited. Any feeling that felt overwhelming, that I struggled to process on my own, I dealt with by distracting myself with food.
This is common.
Research shows that people who have a hard time regulating their emotions are more likely to binge eat.3
Add to that, binge eating episodes are often triggered by uncomfortable emotions—and eating can provide relief from them (at least temporarily).3
Learning to cope with strong emotions is often an important objective when it comes to recovery from compulsive eating.
Personally, when I removed food as a coping mechanism, I felt flooded with emotion. To manage, I mostly turned to journaling. I always felt a release when I wrote down my feelings and thoughts.
For me, it felt important to find an activity that felt distracting enough that I didn’t feel as compelled to eat, but not so consuming that I couldn’t also feel my feelings as they passed through me.
Through this habit, I learned how to communicate with myself again.
Instead of eating-for-all-occasions, I learned when to journal, when to go for a bike ride around my city, when to re-organize my sock drawer, when to cry, and when to invite a girlfriend out for a sloppy night of dancing.
My life got bigger, greater, more joyful, more supported, more meaningful, and finally, “full.”
Try it yourself
For her clients who struggle with emotional eating, Broxterman developed a clever tool called “The Unmet Needs Exercise.”
It helps build awareness between your emotional triggers and your urges to eat, and encourages you to develop more productive coping mechanisms.
Here’s how to do it:
The next time you feel a strong compulsion to eat that’s not due to physical hunger, take a minute to identify what you’re feeling.
If you have trouble articulating your feelings, check out the feelings wheel image below. Start at the center with the broadest emotion you can identify, and work your way outwards to get more specific.
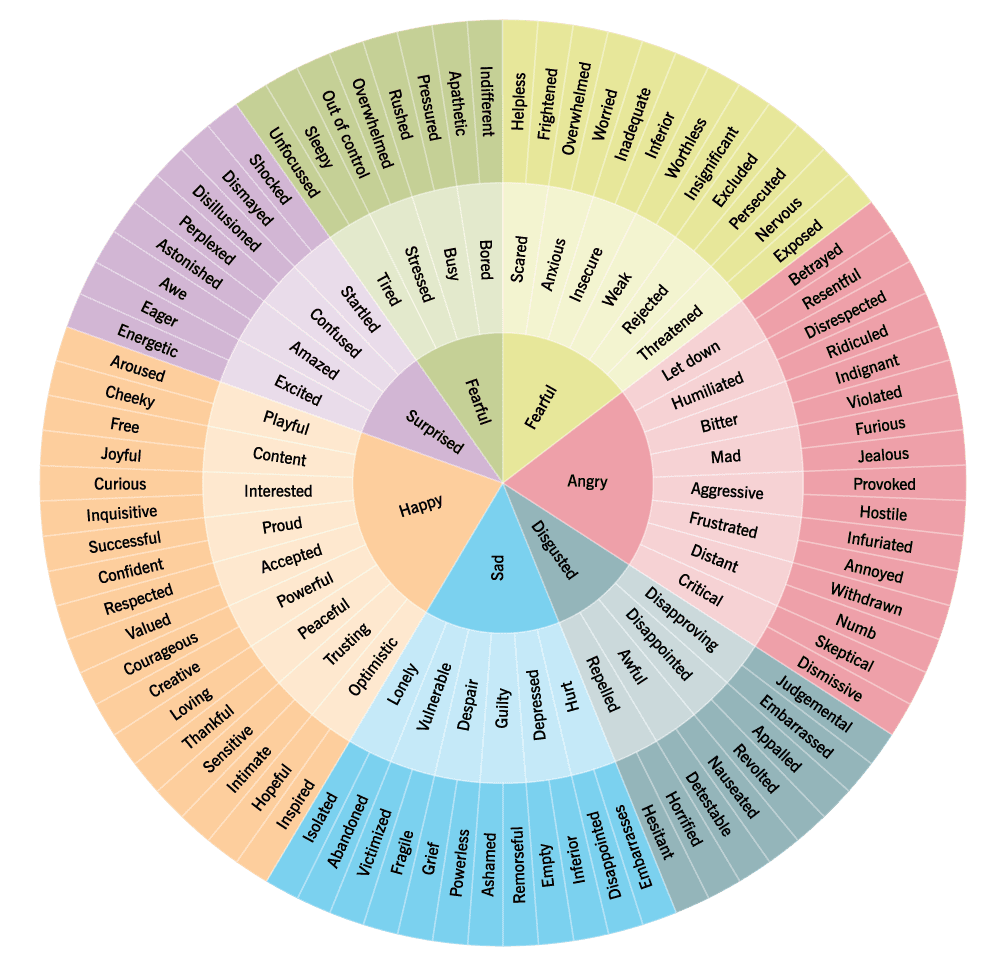
Then, ask yourself: “What is this feeling trying to tell me?”
You can use Broxterman’s image below to guide you, but ultimately you want to figure out what unique needs YOUR feelings are trying to express, plus how you might satisfy that need.
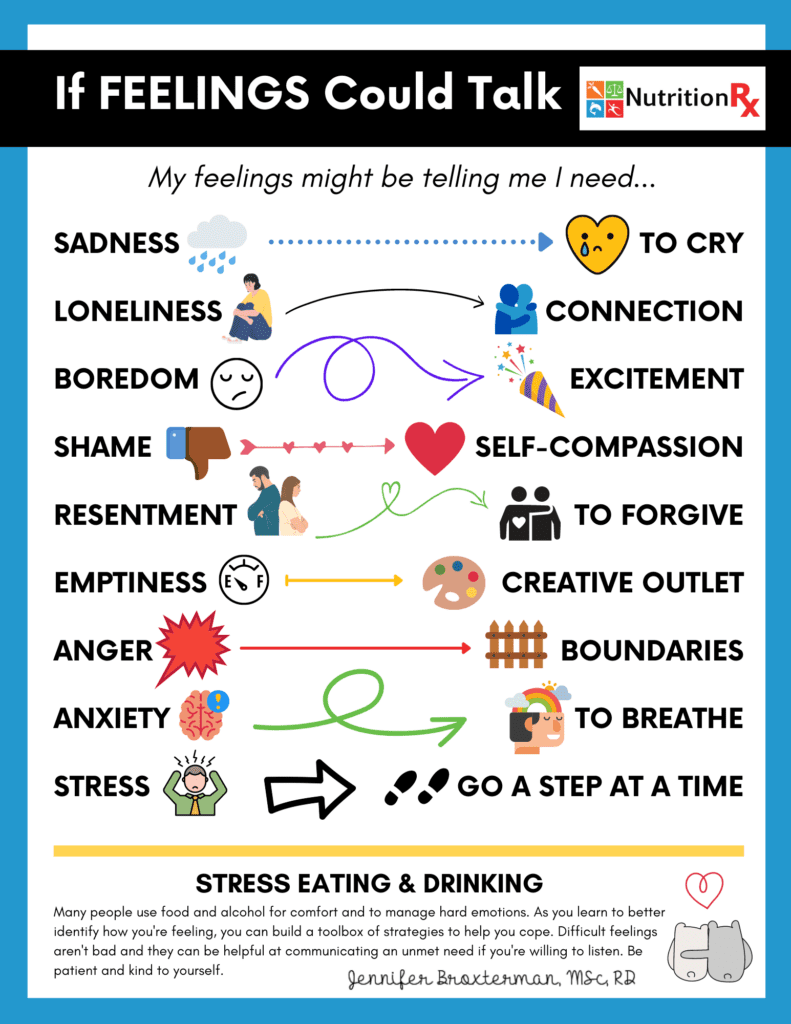
For example, if you identify that you feel bored, and that boredom is telling you that you miss having fun with your friends, try calling or texting a friend, or planning a fun event in the next week.
Then, see how it makes you feel.
This isn’t an immediate fix, but over time, you’ll develop a deeper understanding of your emotional needs, and a broader toolbox of coping strategies.
Step #5: I learned (and practiced) self-compassion.
Shaming and criticizing myself into changing didn’t work.
What did?
Love.
Barf, I know.
But it’s true: The “source” I came to rely on to fuel my progress was a deep desire to be kind, encouraging, and caring to myself.
This is also called self-compassion.
Where my instinct was vicious self-criticism and disgust, I gradually aimed to replace it with understanding and kindness.
I went from saying things like…
“Why are you such a screw-up? Are you NEVER going to get a hold of yourself??”
…to things like…
“Man, I’m sorry this sucks so hard. But I’m going to be here by your side while we figure this out.”
(Which “voice” do you think made me feel more hopeful, less stressed, and more capable of change?)
When I looked at my body, I tried to remove the label of “good” or “bad,” and just focus on the fact of it: I had a body. It carried me around. It held my internal organs in. It was arranged in a certain way, today.
As I regularly pivoted to self-compassion whenever I struggled, my relationship to myself changed.
Instead of a punching bag, my body became something closer to a pet. A loyal dog that I genuinely wanted to feed and walk and not unduly stress. Maybe even give a pat on the head every once in a while.
Try it yourself
Research shows that self-compassion actually plays a critical role in the emergence of eating disorders, as well as the recovery from them.
Lower levels of self-compassion—and higher levels of its counterpart, self-criticism—are associated with4, 5, 6, 7, 8:
- More shame, guilt, self-blame, and negative emotions like anxiety
- A higher likelihood of developing an eating disorder
- Poorer response to eating disorder treatment
- Lower motivation to make positive changes
Meanwhile, higher levels of self-compassion are associated with9, 6, 10:
- Increased appreciation and esteem of one’s body
- Intuitive eating, and less restrictive eating
- Better eating habits and healthier food choices
- A higher tolerance for stress
- Lower rates of depression and anxiety
If you can’t look at yourself without a scowl, self-compassion can be trained, like a muscle. And the more you practice compassionate responses to your own suffering, the more automatic this kind and supportive reflex will become.
Rather than spell it out here, we’ve got a handy self-compassion resource you can practice yourself—or print out for clients. Check it out: Self-Compassion Quickie
Step #6: I sought ongoing support.
After I told my classmate Sarah, I began opening up to others (slowly). I started seeing a therapist, told a few other friends.
Interestingly, I felt the most resistance telling my closest friends and family members.
In my social circle, I was long seen as “the healthy one.” I worried that if I told those people what I was going through, I would disappoint them. Maybe they’d even think I was a fraud. (“You’re not healthy after all!”)
This of course only intensified my shame when my private behaviors didn’t align with the image I knew people associated with me.
Despite my instinct to hide, I began attending group therapy for women with eating disorders. Group therapy was difficult—but it was also a relief to meet other people who really “got it.”
According to Maharaj, talking about your challenges in a supportive group setting can really accelerate progress.
“We’re way more resilient and able to be self-compassionate when we have social support,” Maharaj says.
“The biggest predictor of someone’s mental health being more positive is if they have social support.”
Mostly, I found group therapy to be incredibly freeing. I saw myself in those other women, and also saw that—while they wrestled with their eating habits—they were still smart, responsible, conscientious, and not broken.
They were more than their eating disorders. They were multi-faceted, complex.
Maybe my eating disorder didn’t have to define me either.
It was gradual, and up-and-down, but over the months of therapy and journaling and talking, my compulsion to numb with food lessened. Even when my cravings were high, I learned how to make it to the next moment, and the next.
I knew I had a life outside my kitchen cupboards, and it was full of adventure.
Try it yourself
Not everyone needs support beyond the informal confiding you might get from a trusted friend or family member.
However, if you feel like you’re having trouble managing your compulsions to overeat, professional help—from a therapist or a therapist-led group—can help.
You can try Googling “eating disorder specialist near me” or “eating disorder group therapy near me,” or simply consult the “Think you might need help?” box at the end of this article.
Because binge eating is often a response to unmanaged stress or strong emotions, some people also find mindfulness and stress management apps to be useful. For a guide to some of the best, read: Can these stress apps transform your life for the better?
Without keeping track of it, I went a year without bingeing.
Then another year.
Then one day, about two years after my last episode, I binged. It was minor compared to my history, but it felt scary to “relapse” after years of relative peace.
Instead of hiding it, I talked about it with my then-boyfriend-now-husband. I used curiosity and compassion to look at what factors might have contributed, and how I might forgive myself and move on.
That was 12 years ago.
(And I’ve been binge-free since.)
What “better” looks like (at least for me).
I still have critical thoughts about my body.
I’ve accepted those might not go away.
I’ve realized—as sad as this may sound—there’s a voice inside me that, like a friend who’s burned me too many times, I just can’t trust.
But I can allow it to be there.
I no longer feel compelled to act on those thoughts—either to restrict food to get my body to a specific shape, or to eat when it no longer feels good.
I feel free to eat what I want.
I don’t feel guilty about treats, and definitely don’t feel ashamed to eat them in public.
Sometimes I overeat, and sometimes I eat purely for comfort.
Turns out, this is part of normal eating.
As long as I stay connected to my genuine desire to take care of myself, I know I can trust my appetite—and myself.
Think you might need help?
In this article, we’ve talked about binge eating as an occasional habit or concern.
Binge eating disorder—a more severe and chronic version of occasional binge eating—requires professional help and is beyond a fitness or nutrition coach’s scope of practice.
However, binge eating disorder is the most common eating disorder in the United States.11 Here’s how to recognize it.
Generally, people with binge eating disorder exhibit three qualities:
- They binge. This means consuming a larger amount of food than other people would be able to consume, usually within a two hour period.
- They feel out of control around food, and often guilty and ashamed after eating.
- They binge regularly—at least once a week for three months—and don’t directly “compensate” for the extra calories by over-exercising, restricting food, or purging (vomiting or using laxatives after eating).
If you—or one of your clients—identify with behaviors above, seek or refer out to the care of a professional, like a family doctor, dietitian, or therapist who specializes in eating disorders.
If you’re a coach, remember that you’re not qualified to diagnose or treat any kind of eating disorder. However, you can encourage your client to seek appropriate care, and continue to be part of their larger support network.
A coach may be a person’s first point of contact when they come to terms with an eating disorder; your support, compassion, and direction matter.
For more information, the following resources can provide support:
For Canadians:
The National Eating Disorder Information Centre (NEDIC)
Toll-Free Helpline: 1-866-633-4220
For Americans:
National Eating Disorders Association
Toll-Free Helpline (Call or Text): 1-800-931-2237
International:
For resources by area: https://www.eatingdisorderhope.com/treatment-for-eating-disorders/international
References
Click here to view the information sources referenced in this article.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification.